GCA: Case by Case
GCA:
Case by Case
Sponsored by Novartis US Medical Affairs
- 10-minute read

Michael Putman, MD, MSCI
Assistant Professor of Medicine, Medical College of Wisconsin
See clinical perspectives from Dr Putman throughout on managing patients with giant cell arteritis (GCA)
Meet the expert
Rheumatologist Dr Michael Putman offers his expert insights on optimizing the management of GCA through the examination of 4 intricate patient cases. He delves into challenges in diagnosing and treating GCA, while underscoring the significance of patient education and shared decision-making.

How would you manage a patient with GCA who is requesting to increase their prednisone dose for new symptoms?
- Sex: Male
- Age: 81 years
Current Presentation
Chief complaints: Hip pain (worsens with corticosteroid tapering) and headaches (respond to acetaminophen)
Clinical History
GCA duration: 8 months
Medications: IL-6 inhibitor and
prednisone (6 mg QD)
Clinical Findings
Examination: Decreased rotation to internal rotation of bilateral hips
Laboratory tests: ESR 7 mm/hr, CRP normal
X-rays: Moderate degenerative arthritis in hips


“Corticosteroids can improve symptoms unrelated to active GCA, including osteoarthritis and benign headache syndromes. A careful history and patient education can help us and our patients differentiate between true GCA symptoms and those of comorbidities that may masquerade as GCA”
95%
Risks associated with corticosteroid therapy include:
Fracture and osteoporosis1-4
Cardiovascular disease1-4
Diabetes mellitus1,3,4
Glaucoma3,4
Infection2,4 and sepsis1
Weight gain4
Cushingoid features4
Differentiating between GCA and aches/pains from comorbid conditions5
Understanding risk of AEs with prolonged corticosteroid use1-4

Explaining rationale and importance of corticosteroid tapering to balance benefit vs AEs5,6

Incorporating physical therapy to address comorbid pain7 and reduce corticosteroid dependence

How would you manage a newly diagnosed patient with GCA with diverticulosis and other comorbidities?

- Sex: Female
- Age: 72 years
Current Presentation
Chief complaints: Daily headaches, jaw claudication, recent left-sided “blurry” vision
Clinical History
Medications: Prednisone (40 mg QD), losartan, and hydrochlorothiazide
- Diverticulosis identified on colonoscopy at 60 years of age
- No history of malignancy or diverticulitis
- History of hyperlipidemia, hypertension, and myocardial infarction at 67 years of age
Clinical Findings
Laboratory tests: ESR 65 mm/hr, CRP 30 mg/L
*Used as off-label treatment option as per ACR guidelines.


“As neither hyperlipidemia nor diverticulosis are contraindications to IL-6 inhibitors, I would favor using targeted therapies over long-term corticosteroid use. Given the long-term risks of corticosteroids, I prefer to taper as soon as is clinically feasible”
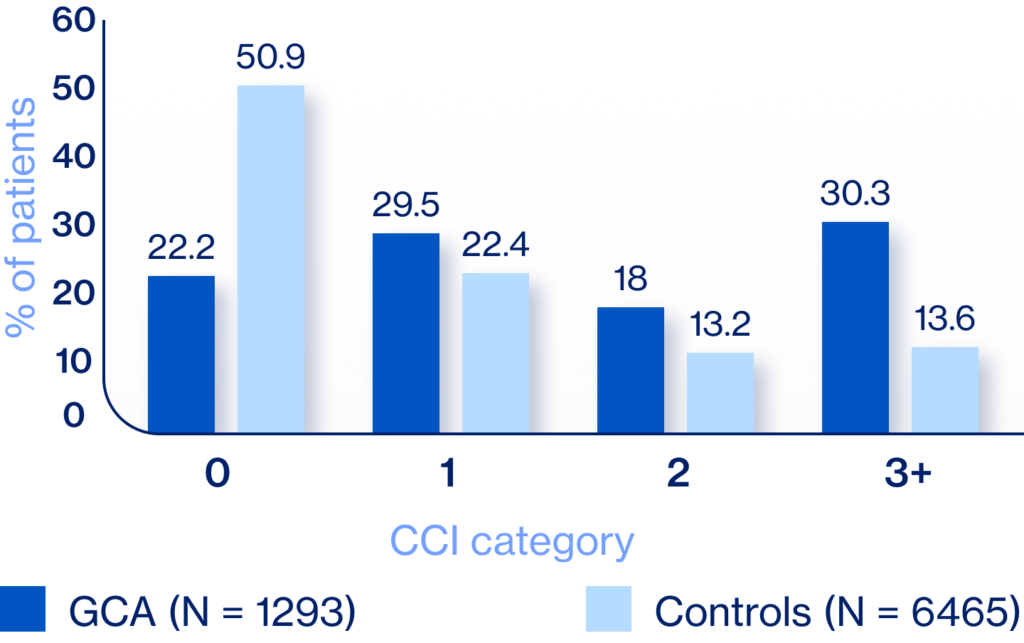
The CCI predicts a patient’s 10-year mortality risk based on the presence and severity of comorbid conditions. Higher scores indicate a higher predicted risk of mortality and increased overall health burden9,10
CCI score at diagnosis for patients with GCA vs controls
ACR guidelines recommend6:
“For patients with newly diagnosed GCA, we conditionally recommend the use of oral corticosteroids with IL-6 inhibitor over oral corticosteroids alone”

What would be your next step when a patient relapses on therapy?

- Sex: Male
- Age: 71 years
Current Presentation
Chief complaints: Sudden vision loss
Clinical History
Medications: IL-6 inhibitor, corticosteroids discontinued 8 months ago
Clinical Findings
Physical exam: Ophthalmology reports “optic disc pallor concerning for recurrent GCA”


“Recurrent vision loss on therapy is rare, but when it happens, it is incredibly challenging. Until recently there was only one FDA-approved therapy for GCA and the strength of evidence for off-label options (per ACR guidelines) is mixed. This highlights the urgent need for additional approved therapies”
Relapses occur in almost half of patients with GCA11
GCA relapse: reappearance of ≥1 GCA symptoms11
- Most are minor12
- Most common <2 years after diagnosis12
- Irreversible ophthalmological or ischemic complications are rare, but can occur12
- Episodes of PMR
- Headache
- Systemic symptoms (eg, fever, anemia)
Generally respond to increased corticosteroid dose
- Severe ischemic complications (eg, permanent loss of vision, stroke)
- Active inflammation leading to structural damage
ACR guidelines recommend6:
“For patients with GCA who experience disease relapse with symptoms of cranial ischemia, we conditionally recommend adding a noncorticosteroid immunosuppressive agent and
increasing the dose of corticosteroids over increasing the dose of corticosteroids alone”

When would you consider differential diagnosis in a patient diagnosed with refractory PMR?

- Sex: Female
- Age: 64 years
Current Presentation
Chief complaints: Persistent fatigue, neck pain, fever
Clinical History
Diagnostic history:
- Initially diagnosed with PMR, started on prednisone (down to 14 mg QD)
- No headaches or jaw claudication
Medications: None currently
Key comorbidities: Hypertension
Clinical Findings
Laboratory tests: ESR 91 mm/hr, CRP 8.3 mg/L


“Large vessel involvement in GCA is often under-recognized and may explain “refractory” PMR. Temporal artery biopsies may be normal for patients with large vessel involvement. In alignment with ACR guidelines, I always image the aorta and its branches (PET-CT preferred) to confirm diagnosis and exclude mimics”
Large vessel involvement of GCA is common and associated with vascular complications such as aortic
aneurysm and large vessel stenosis13

Large vessel
involvement
present in up to 83% of patients with GCA;13-15 can occur with or without cranial GCA13

Aortic aneurysm risk
increased 17-fold for patients with GCA vs age/sex matched comparators16

Risk of death
increased 3.4-fold for patients with aortic aneurysm vs those without large vessel involvement17
Noninvasive imaging may improve diagnosis and
monitoring of large vessel GCA13

ACR guidelines recommend6:
“For patients with suspected GCA and a negative temporal artery biopsy result (or results), we conditionally recommend noninvasive vascular imaging of the large vessels with clinical assessment to aid in diagnosis over clinical assessment alone”

What is needed to improve standards of care in GCA?
Corticosteroid-sparing therapies with an acceptable balance of efficacy and toxicity1
Agents targeting varied disease pathways2 offer flexible options for evolving patient needs18
Approved treatments with a reduced risk of relapse,1 particularly for patients not controlled on current therapies18
Continued innovation is critical to expand therapeutic options, optimize patient outcomes, and improve standards of care in GCA
ACR, American College of Rheumatology; AE, adverse event; CRP, C-reactive protein; CTA, computed tomography angiography; ESR, erythrocyte sedimentation rate; FDA, Food and Drug Administration; GCA, giant cell arteritis; IL, interleukin; LDL-C, low-density lipoprotein cholesterol; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; PET-CT, positron emission tomography and computed tomography; PMR, polymyalgia rheumatica; QD, once daily.
1. Low C, Conway R. Ther Adv Musculoskel Dis. 2019;11:1759720X19827222. 2. Mollan SP et al. Eye (Lond). 2021;35(3):699-701. 3. Hellmich B et al. Ann Rheum Dis. 2020;79(1):19-30. 4. Buttgereit F
et al. Rheumatology. 2018;57(suppl. 2):ii11-ii21. 5. Dejaco C et al. Ann Rheum Dis 2024;83(1):48-57. 6. Maz M et al. Arthritis Rheumatol. 2021;73(8):1349-1365. 7. Kolasinski S et al. Arthritis Care Res (Hoboken). 2020;72(2):149-162. 8. Babigumira JB et al. Rheumatol Ther. 2017;4(1):111-119.
9. Charlson ME et al. J Chron Dis. 1987;40(5):373-383. 10. Deyo RA et al. J Clin Epidemiol. 1992;45(6):613-619. 11. Aussedat M et al. Autoimmun Rev. 2022;21(1):102930.
12. Alba MA et al. Autoimmun Rev. 2024;23(6):103580. 13. Koster MJ, Matteson EL, Warrington KJ. Rheumatology. 2018;57(suppl_2):ii32-ii42. 14. Blockmans D et al. Arthritis Rheum.
2006;55(1):131-137. 15. Prieto-González S et al. Ann Rheum Dis. 2012;71(7):1170-1176
16. Evans JM et al. Ann Intern Med. 1995;122(7):502-507. 17. Kermani TA et al. Ann Rheum Dis. 2013;72(12):1989-1994. 18. Galli E et al. Curr Opin Rheumatol. 2024;36(5):344-350.