Debunked.
Expert perspectives on Sjögren’s Disease myths
Sponsored by Novartis US Medical Affairs
- 10-minute read and listen

Sjögren’s Disease: Beyond Sicca
Sara McCoy, MD, PhD
Click on the audio clips throughout to hear clinical perspectives from Dr McCoy
Test your knowledge
True or False?
- Sara McCoy, MD, PhD
Hello! My name is Sara McCoy, and I’m an assistant professor of rheumatology and the director of the University of Wisconsin Health Sjögren’s clinic. Thank you so much for joining me for this Therapeutic Update sponsored by Novartis US Medical Affairs. I have been compensated to participate in this program where we will discuss six myths in Sjögren’s disease. If you scroll to the bottom of this page, you can download a visual summary of the content we’ll cover today, along with a full transcript of this discussion. To get started, click next to jump to the first Sjögren’s disease myth to learn more.
1
Myth: Sicca in patients with Sjögren's disease is localized and does not significantly impact patients’ daily lives
Reality
Although Sjögren’s disease is primarily associated with dysfunction of the salivary and lacrimal glands, sicca, or dryness in Sjögren’s disease, can be systemic, occurring in the eyes, mouth, upper respiratory tract, skin, and vagina. It can also be debilitating, significantly impacting patient quality of life1-5
Nearly 1 in 3
patients with Sjögren's disease experience vaginal dryness6
Nearly
1 in 3
patients with Sjögren's disease experience vaginal dryness6
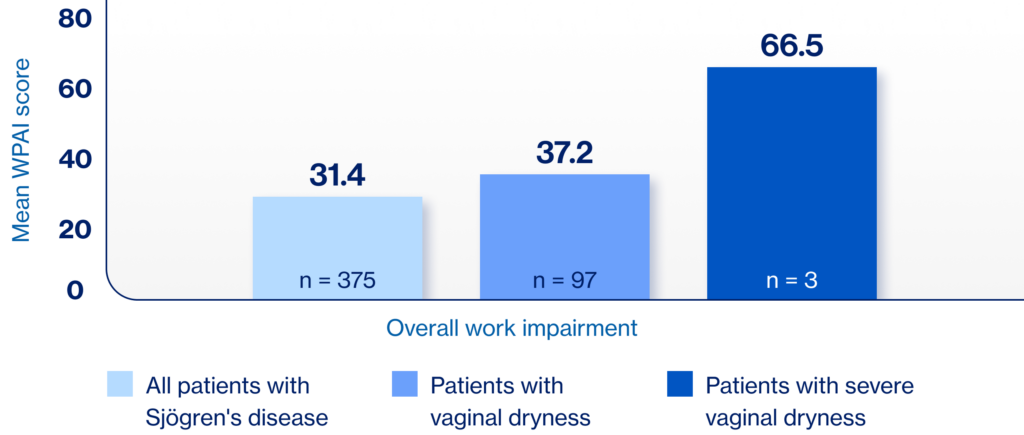
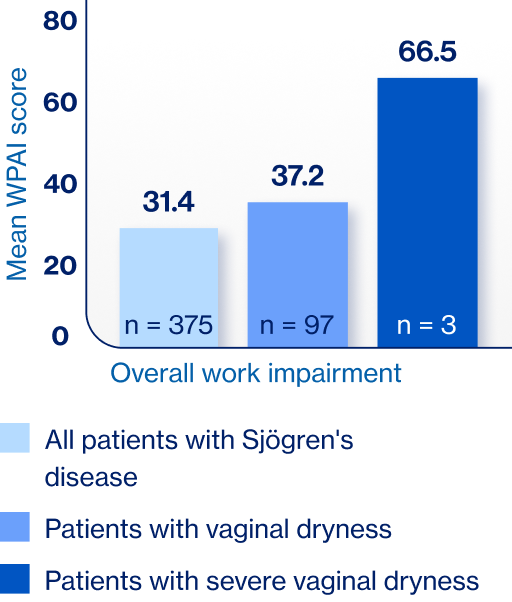
Work impairment is higher in patients with Sjögren’s disease and vaginal dryness compared to patients with Sjögren’s disease without vaginal dryness6,*

- Sara McCoy, MD, PhD
Is sicca, or dryness, in patients with Sjögren’s disease localized and not impactful to patients’ daily lives? While it’s true that over 90% of patients have sicca of the eyes, mouth, or both, it’s important to recognize that dryness in patients with Sjögren’s can actually occur throughout the body.1,2 In fact, many of our patients experience dryness of the skin, upper respiratory tract, and vagina.3 I think it’s important for us to realize that these symptoms can be debilitating for our patients and have a significant impact on patient quality of life.1,4-8 Not only do I see the burden that Sjögren’s can take on my patients but also my colleagues and I published a paper that surveyed patients with Sjögren’s in the United States.1 The top two symptoms that patients experienced were dry eye and dry mouth.1 These patients also reported significant impacts to aspects of their quality of life including their sex life, participating in hobbies, and in their careers.1
I also want to come back to something I said earlier, that sicca in Sjögren’s can occur throughout the body. In particular, vaginal dryness can occur in nearly 1 in 3 patients with Sjögren’s,9,10 and it’s one that doesn’t get enough attention in my opinion. My colleagues and I recently published a study that showed vaginal dryness can impact patient quality of life, fatigue, work productivity, and activity impairment.9 We showed that as vaginal dryness severity increases, these patient recorded outcomes I just mentioned got worse.9 For example, in our study, we collected data on overall work productivity and activity from 375 patients with Sjogren’s.9 The total work productivity lost was 31.4%; this increased to 37.2% in patients with any vaginal dryness or to 66.5% in patients with severe vaginal dryness, really highlighting the substantial impact dryness can have on patients.9,10 Because vaginal dryness is so common and can affect quality of life in patients, I include one screening question in my review of systems for my female patients to ask about this. If the response is positive, I have a guide on management I provide to patients as well as free samples of agents we can use to help ameliorate the dryness.
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
2
Myth: Sjögren's is a syndrome just characterized by ocular and oral sicca
Reality
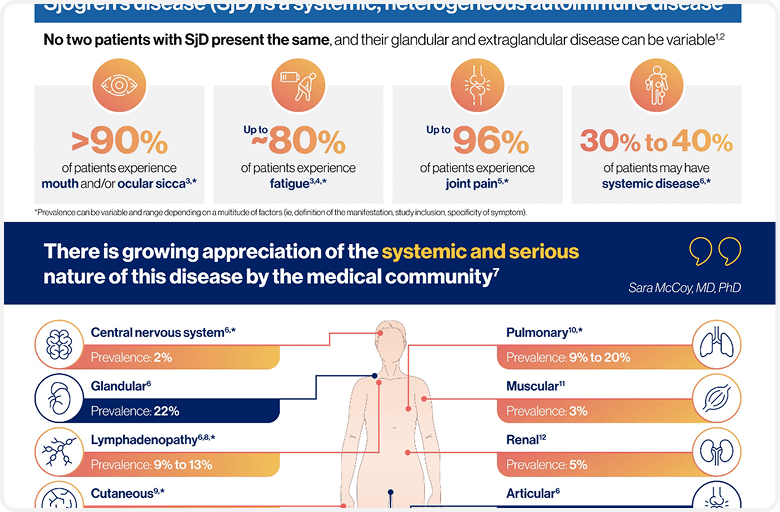
Sjögren’s disease is more than sicca symptoms, it is a serious, systemic, heterogeneous, autoimmune disease. An assessment of patients with Sjögren’s disease should go beyond dryness and include screening for systemic complications, including those of the joints, skin, and lymph nodes7
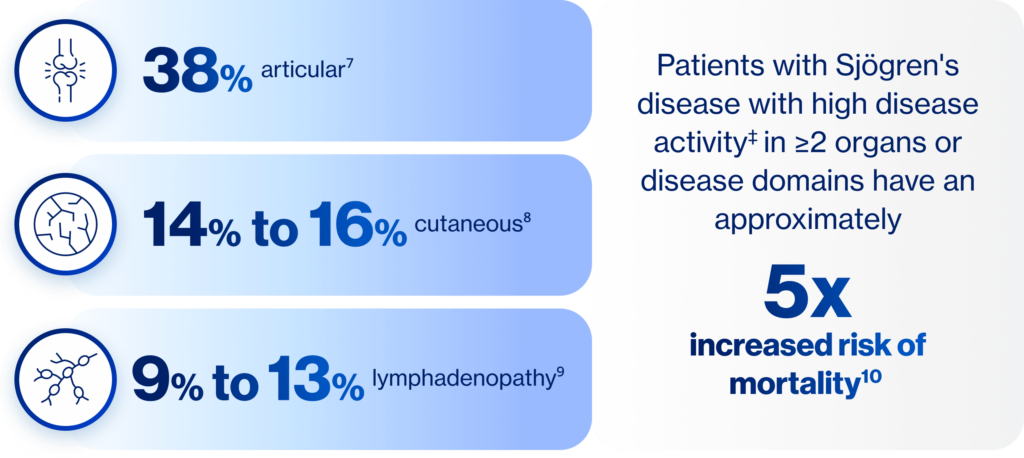
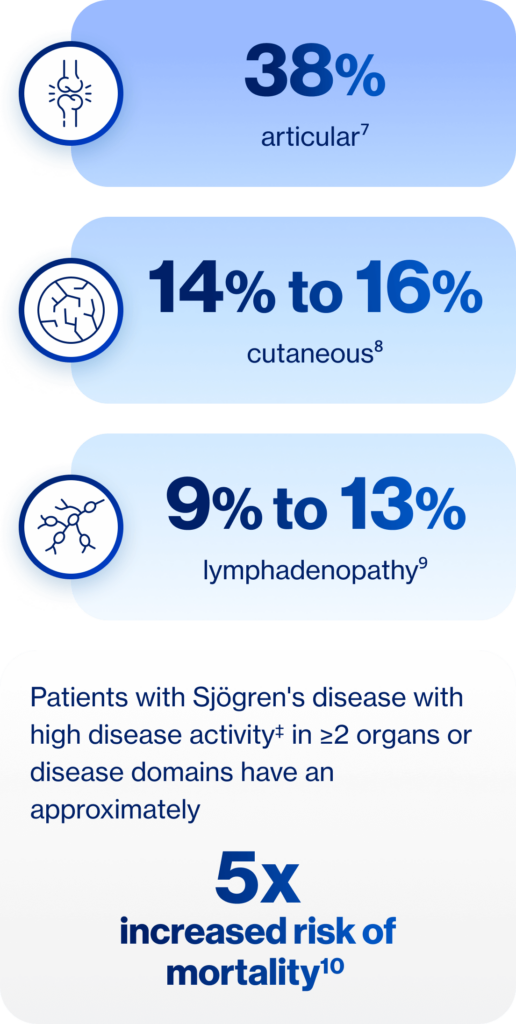
‡Systemic activity according to the number of clinESSDAI domains classified as high activity at diagnosis.

- Sara McCoy, MD, PhD
There is a myth that when you have a patient with Sjögren’s in front of you, you should primarily focus on assessment of their dryness. While it is certainly true that dryness is an important part of our clinical assessment, the reality is that Sjögren’s is more than dryness – it is a systemic, heterogeneous autoimmune disease.2,11,12 So, if I have a patient with Sjögren’s in front of me, my assessment also needs to include monitoring for systemic disease, and may include areas that are routinely assessed such as the joints, glands, lymph nodes, and skin.13 While current literature and our clinical experience tell us that the prevalence of systemic manifestations varies, we also know there is an increased risk of mortality in patients with high systemic disease activity.2,13,14 When I have a patient with Sjögren’s in front of me, I take a systemic approach to their exam. We discuss constitutional symptoms such as fevers, night sweats, and unintentional weight loss. I look for salivary gland enlargement, arthritis, and rash. We discuss if they have had any chest pain, shortness of breath, neuropathic symptoms. I also perform labs to evaluate the kidneys, blood counts to look for lymphoma risk, and their overall immune activity. Depending on these outcomes, I have a low threshold to perform pulmonary function tests and CT of the chest to evaluate for pulmonary involvement.
Let’s also discuss the myth that Sjögren’s is a syndrome. We know that language matters and Sjögren’s should no longer be referred to as a syndrome but as a disease. And this is not just my clinical opinion – there is growing appreciation of the systemic and serious nature of this disease by the medical community. This is best illustrated by the recent adoption of the nomenclature change from syndrome to disease in Sjögren’s.15 This was a patient-initiated change that was voted on and officially adopted by the entire international Sjögren’s community.15 Thus, the community at large respects the severity of Sjögren’s disease and the fact there is a clear pathologic process driving patients’ symptoms. Additionally, the multifaceted aspect of Sjögren’s disease outside of dry eye and dry mouth is reflected by the ESSDAI. The ESSDAI assesses 12 organ domains and is endorsed by regulatory agencies as the primary outcome in most ongoing Sjögren’s clinical trials.16 The ESSDAI comprises organ involvement we know is specific to Sjögren’s disease, including domains associated with major morbidity and mortality. Each domain is centered around an organ system and each system is weighted based on the severity of the specific manifestation.16 Here are some examples: persistent cough due to bronchial involvement without clear radiographic abnormalities that is attributed to Sjögren’s disease is considered mild, whereas severe interstitial lung disease with significant pulmonary function test abnormalities would be weighted heavily. This composite score attempts to capture the wide range of organ involvement and severity that is seen in Sjögren’s disease.16
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
3
Myth: Sicca symptoms always precede systemic disease
Reality
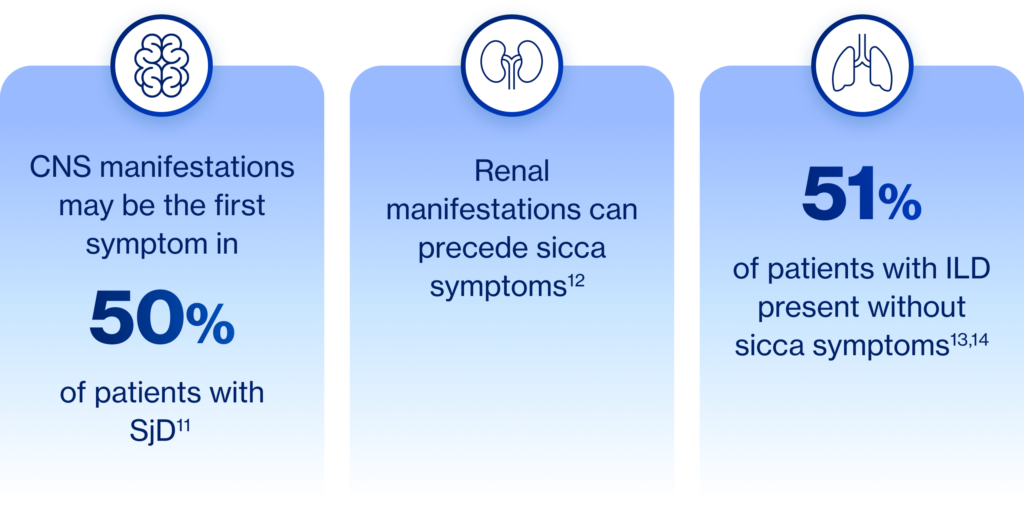
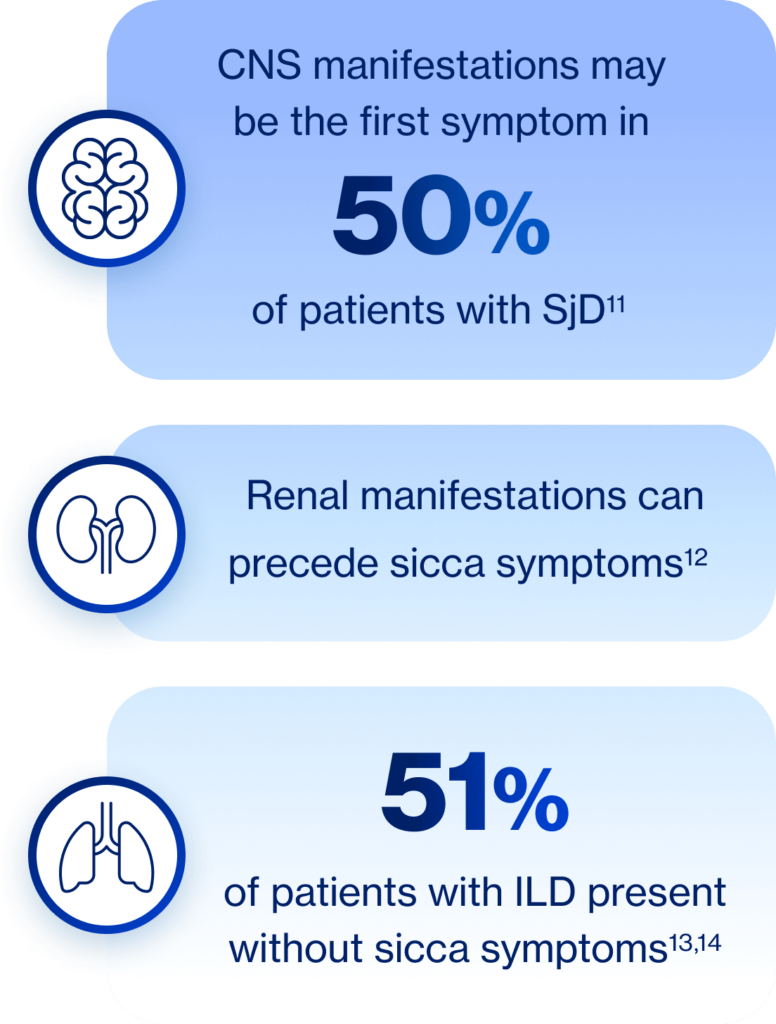
Patients with Sjögren’s disease may present with systemic disease that precedes sicca symptoms11-14

- Sara McCoy, MD, PhD
As most of us think of Sjögren’s as a sicca disease, we may also be inclined to think that those symptoms always present first. We may be most familiar with our patients coming to us with ocular or oral sicca as their first noticeable symptoms, but systemic disease can emerge first, even if Sjögren’s disease isn’t top of mind as a possible cause.17-20 For example, respiratory symptoms such as dry cough may precede a Sjögren’s disease diagnosis by about 2 years.21 I actually have a patient in my practice, a 78-year-old male, who was referred to me with a diagnosis of pulmonary fibrosis and was experiencing increased respiratory needs and a productive cough. He had no xerophthalmia or xerostomia, but upon further evaluation, he was diagnosed with Sjögren’s disease.22 I find anecdotally that patients with more severe disease might not endorse the same level of symptoms, thus one needs to keep in mind Sjögren’s disease in the appropriate clinical context despite the lack of symptoms. This is further reinforced in the literature and my own studies where patients with lower symptom burden can actually have a discordant increase in objective extraglandular organ involvement. Other manifestations can also precede symptom onset including gastrointestinal and renal complications, which are two others that I always keep in mind when evaluating patients.18,23
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
4
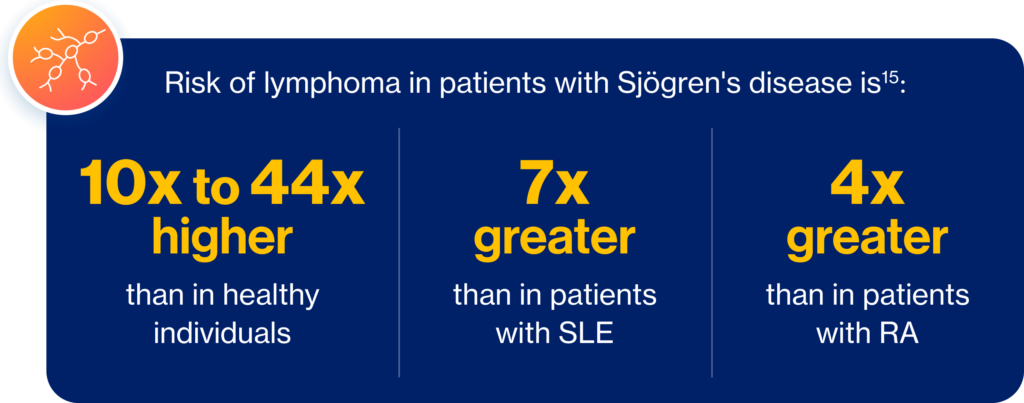
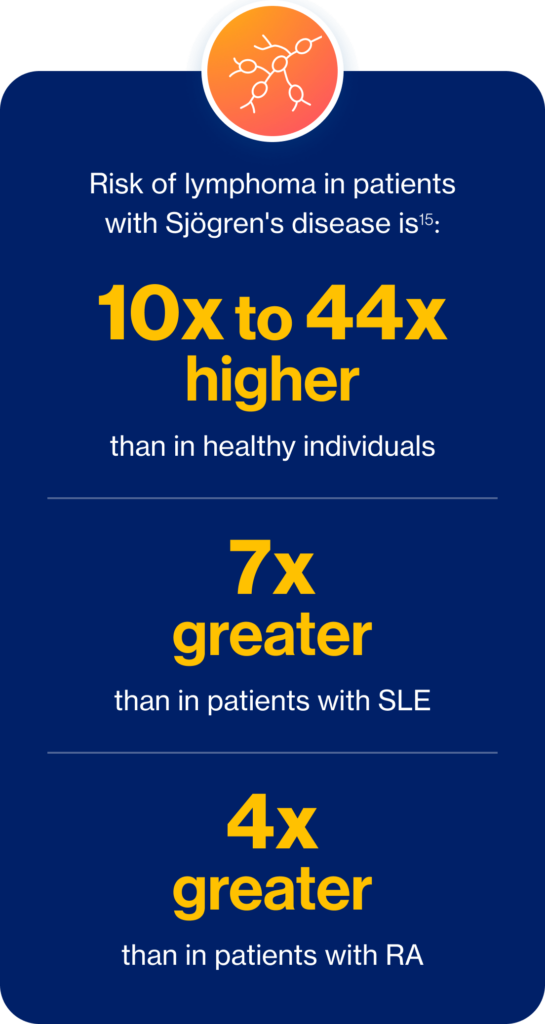
Myth: Lymphoma is uncommon in patients with Sjögren's disease
Reality
Complications of Sjögren’s disease can be serious and life-threatening and are associated with a significantly increased risk for mortality and lymphoma10,15

- Sara McCoy, MD, PhD
Lymphoma is uncommon in patients with Sjögren’s disease – this is a myth. The reality is that lymphoma is an important systemic complication of Sjögren’s disease. The risk for lymphoma can range, depending on the publication, from 10 to 44 times increased risk in patients with Sjögren’s compared to the general population.24 One meta-analysis found the overall risk for non-Hodgkin’s lymphoma in patients with Sjögren’s to be approximately 14 times higher than in the general population.25 Mucosa-associated lymphoid tissue, or MALT lymphoma of the gland is the most common lymphoma in Sjögren’s disease.26 This is important to consider as the risk for lymphoma in patients with Sjögren’s is approximately four times higher than in patients with rheumatoid arthritis.24 Furthermore, this is one of the major concerns of our patients with Sjögren’s disease.1
This highlights the importance of assessing lymphoma risk in our patients. To screen for lymphoma, I evaluate constitutional symptoms and gland and lymph node enlargement on ROS, or review of systems. On exam, I look for glandular enlargement, splenomegaly, and evidence of leukocytoclastic vasculitis. I do an ultrasound of the salivary glands; a CBC with diff to identify patients who are neutropenic; serum protein electrophoresis; beta-2 microglobulin; and lactate dehydrogenase, I also look for elevated rheumatoid factor, cryoglobulins, and low complement. Presence of these and other risk factors, such as SSA positivity, salivary gland enlargement, and Raynaud’s phenomenon, can increase the risk for lymphoma development.27 I know it’s not always appreciated, but I want to emphasize that the complications of Sjögren’s disease can be serious and life-threatening in patients with risk factors.
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
5
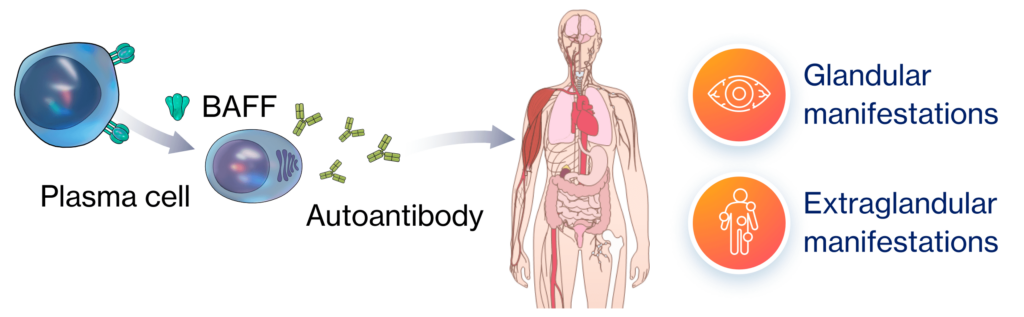
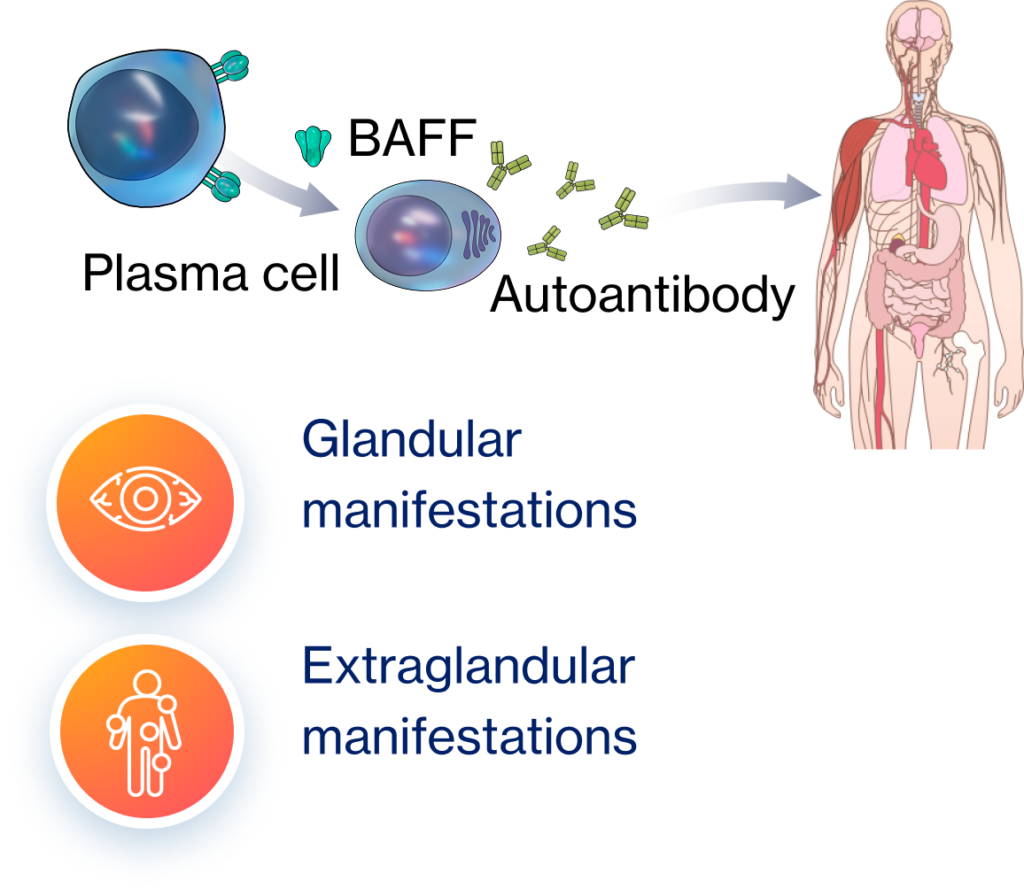
Myth: Hyperactive B cells are only found in glandular tissue in Sjögren's disease
Reality
Sjögren’s disease is a systemic B-cell–driven autoimmune disease where hyperactive B cells drive chronic inflammation and damage throughout the body, resulting in glandular and extraglandular manifestations7,16-20

- Sara McCoy, MD, PhD
Though most people associate B cells with Sjögren’s disease, it may not be fully appreciated that hyperactive B cells are the hallmark of the disease and drive inflammation and damage to the glandular tissue and throughout the rest of the body, resulting in extraglandular manifestations.2,28-32 In Sjögren’s, we have this pathological cycle of immune activation that’s driven by the perpetual activation of B cells, which leads to chronic inflammation and potentially irreversible, systemic tissue destruction.28,29 In the exocrine glands, it might cause destruction of the epithelium and decreased tear and saliva production, which causes the characteristic Sjögren’s dryness symptoms we’re familiar with. But pathogenic B cells can also infiltrate extraglandular tissues, triggering systemic inflammation and tissue damage.2,28-32
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
6
Myth: There are approved disease-modifying therapies for Sjögren's disease
Reality
There are no FDA-approved disease-modifying drugs for Sjögren’s disease. There is a need to improve standards of care, as current management is inadequate, does not address systemic complications, and provides only partial and symptomatic relief21-23

Systemic treatments have demonstrated limited improvements in systemic disease outcomes21,24,25
97%
of patients somewhat or strongly agree that they wish there were better treatments available for Sjögren's disease26,*

- Sara McCoy, MD, PhD
Are there any FDA-approved disease-modifying therapies for Sjögren’s disease that have demonstrated systemic and symptomatic efficacy? Unfortunately, there are not, meaning any systemic immunosuppressive treatments used for Sjögren’s disease are off-label. Therefore, our current Sjögren’s management approach is focused on relieving dryness symptoms with secretagogues that can be challenging for our patients to adhere to. They provide only temporary relief, so they require frequent dosing and can be costly.11,13,33 Patients are advised to increase water intake, use salivary substitutes, chewing gum or sugar-free mints. However, a Cochrane systematic review found that no specific topical therapy is more effective at treating dry mouth than any other, and agents that use sugar-free substances commonly cause adverse GI effects.34 Cholinergic agonists frequently cause diaphoresis or GI upset and are associated with a failure rate of 30 to 50%.35,36 When it comes to systemic therapies, glucocorticoids are frequently used, but evidence for their use is limited, and there are risks for long-term adverse events. Though hydroxychloroquine and rituximab, two other systemic therapies, are included in Sjögren’s guidelines, they have failed in clinical trials to demonstrate improvement on both systemic disease and symptomatic outcomes.13,37,38 Ultimately, we know that our patients wish there were better treatments available for Sjögren’s.39 In a survey of 3622 patients conducted by the Sjögren’s foundation, 97% of patients reported that better treatments for Sjögren’s are needed.39 Our patients with Sjögren’s face significant burdens, impacts on their overall quality of life, and on activities of daily living due to their disease, so an improvement in standards of care is needed and one of the top desires of our patients. I want to thank you for joining me today as we’ve discussed Sjögren’s disease myths. I hope you’ve learned something along the way. Remember to download our visual summary from the top of the page.
1. McCoy S et al. Clin Rheumatol. 2022;41:2071-20787. 2. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 3. Mavragani CP, Moutsopoulos HM. CMAJ. 2014;186:E579-E586. 4. Parisis D et al. J Clin Med. 2020;9(7):2299. 5. McCoy SS et al. J Rheumatol. 2021;48(7):1029-1036. 6. Perella C et al. Rheumatol Ther. 2023;10:601-614. 7. Kassan SS, Moutsopoulos HM. Arch Intern Med. 2004;164(12):1275-1284. 8. Saldanha J et al. Am J Ophthalmol 2020;219:40-48. 9. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 10. van Nimwegen JF et al. Rheumatology (Oxford). 2015;54(7):1286-1293. 11. Vitali C et al. Front Med (Lausanne). 2021;8:676885.
12. Ter Borg EJ, Kelder JC. Rheumatol Int. 2017;37(7):1153-1158. 13. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 14. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 15. Sjögren’s Foundation. Accessed April 1, 2025. https://sjogrens.org/blog/2024/language-matters-the-international-sjogrens-community-changes-sjogrens-syndrome-to 16. Seror R et al. RMD Open. 2015;1(1):e000022. 17. Moreira L et al. Rheum Int. 2015;35:289-294. 18. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 19. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 20. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 21. Flament T et al. Eur Respir Rev. 2016;25(140) 110-123. 22. Unpublished case study provided courtesy of Dr Sara McCoy.
23. Kim-Lee C et al. Springerplus. 2015;4:766. 24. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 25. Liang Y et al. Ann Rheum Dis. 2014;73(6):1151-1160. 26. Papageorgiou A et al. PloS One. 2015;10(2):e0116189. 27. Fragkioudaki S et al. Medicine (Baltimore). 2016;95(25):e3766.
28. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 29. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-14. 30. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 31. Du W et al. Front Immunol. 2021;12:684999. 32. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491.
33. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 34. Brito-Zerón P et al. RMD Open. 2019;5:e001064. 35. Gil-Montoya J-A et al. Med Oral Patol Oral Cir Bucal. 2016;21(3):e355-366. 36. Farag AM et al. Oral Dis. 2019;25(8):1937-1944. 37. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 38. Gottenberg JE et al. JAMA. 2014 312(3):249-258. 39. Sjögren’s Foundation. Living with Sjogren’s. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf.
Downloadable resources
View our visual summary of the key facts you need to know about Sjögren's disease
View our visual summary of the key facts you need to know about Sjögren's disease

1. Parisis D et al. J Clin Med. 2020;9(7):2299. 2. McCoy S et al. J Rheumatol. 2021;48(7):1029-1036. 3. Perella C et al. Rheumatol Ther. 2023;10:601-614. 4. McCoy S et al. Clin Rheumatol. 2022;41:2071-2078. 5. Saldanha J et al. Am J Ophthalmol. 2020;219:40-48. 6. McCoy S et al. Poster presented at: American College of Rheumatology Convergence 2023; November 10-15, 2023; San Diego, CA. Abstract 2179. 7. Mariette X, Criswell LA. N Engl J Med. 2018;378:931-939. 8. Andre F, Bockle BC. J Dtsch Dermatol Ges. 2022;20:980-1002. 9. Stergiou IE et al. Clin Exp Rheumatol. 2022;40:2357-2362. 10. Brito-Zerón P et al. eClinicalMedicine. 2023;61:102062. 11. Moreira L et al. Rheum Int. 2015;35:289-294. 12. Aiyegbusi O et al. Rheumatol Ther. 2021;8:63-80. 13. Gao H et al. Int J Rheum Dis. 2018;21(7):1423-1429. 14. Sambataro G et al. Autoimmun Rev. 2020;19:102447. 15. Huo R et al. Open Med (Wars). 2023;18(1):20230829. 16. Verstappen GM et al. Nat Rev Rheumatol. 2021;17(6):333-348. 17. Nocturne G, Mariette X. Nat Rev Rheumatol. 2018;14:133-145. 18. Negrini S et al. Clin Exp Med. 2022;22(1):9-25. 19. Du W et al. Front Immunol. 2021;12:684999. 20. Baldini C et al. Nat Rev Rheumatol. 2024;20:473-491. 21. Ramos-Casals M et al. Ann Rheum Dis. 2020;79:3-18. 22. Birt JA et al. Clin Exp Rheumatol. 2017;35(1):98-107. 23. Vitali C et al. Front Med (Lausanne). 2021;8:676885. 24. Devauchelle-Pensec V et al. Ann Intern Med. 2014;160(4):233-242. 25. Gottenberg JE et al. JAMA. 2014; 312(3):249-258. 26. Sjögren’s Foundation. Accessed February 18, 2025. https://sjogrens.org/sites/default/files/inline-files/LivingwithSjogrens-8.5×11-2022-Mar31_7pm.pdf
Novartis has paid RheumNow to host this content. Novartis is solely responsible for all the written content within this presentation.