
Treatment goals for RA: Is it time to transition MOAs?
- 16-minute listen
Rheumatologists Dr. Christina Charles-Schoeman and Dr. Manish Jain discuss their approaches to setting and pursuing treatment goals for patients with poorly controlled RA after TNFis
Podcast

- Dr. Andrea Rubbert-Roth • March 2025
The experts

Christina Charles-Schoeman, MD, MS
Professor of Medicine
Chief of the Division of Rheumatology
UCLA Health
Los Angeles, CA

Manish Jain, MD
Attending Physician Ravenswood Rheumatology Chicago, IL
What would you do?

Patient A
- Longstanding erosive RA
- Did not achieve LDA/remission after >3 years of TNFi + MTX treatment
- Recent diabetes diagnosis
How would you treat Patient A?
If your patients have uncontrolled RA, their disease may be progressing

Loss of physical function and quality of life1–3
Socioeconomic and psychological burden4–7
Comorbidity risk
(CVD,4,8,9 infection,10,11 malignancy4,12)
Review the data on disease duration and remission:
In the podcast, Dr. Charles-Schoeman discussed this study on the relationship between disease duration and the achievement of remission
Every patient deserves to
achieve disease control
Monitor disease regularly
ACR guidelines recommend13:
Frequent monitoring of disease activity using validated instruments
Evaluate current treatment
ACR guidelines recommend13:
In the absence of improvement, reevaluate therapy within 3 months
If your patient is not achieving disease control, consider a change in treatment
ACR guidelines recommend13,*:
Switching to a treatment of a different class over cycling treatments of the same class
Explore the full ACR guidelines
Read more about the latest RA guidelines
Review real-world data
In the podcast, Dr. Charles-Schoeman discussed this study on real-world disease monitoring and treatment reevaluation
Could a switch in MOAs after TNFi failure bring your patients closer to their treatment goals?
probability that MOA switch is better
probability that MOA switch is better
than TNFi cycling after first-line TNFi failure†
Improved DAS28 remission may include improvements in20:
Swollen joint count
Tender joint count
Patient’s global health (VAS)
Review the full study here, including a meta-analysis of other disease outcomes (ACR response, treatment withdrawal, etc.)
Study details: The network meta-analysis comprised RCTs and observational studies identified via a literature search in 2018. To account for the wide range of study populations and designs, the results presented are from two models to conduct the network meta-analysis: fixed-effect or Bayesian hierarchical. The authors determined the model presented for the primary results of each outcome (above) based on the deviance information criterion.
†Analysis using a Bayesian hierarchical network meta-analysis of five RCTs.
Additionally, patients who switched MOA have been observed to be:
Less likely to change treatments again15
More likely to adhere to treatment16
More data on TNFi cycling vs MOA switching is coming soon:
SUNSTAR (NCT03227419)
ABA vs TCZ in TNFi-IR patients with RA
ADDORA-switch (NCT04251741)
TNFi vs non-TNFi after ADA failure based on ADA serum concentration
SELECT-SWITCH (NCT05814627)
UPA vs ADA in TNFi-IR patients with RA
Your patients deserve the opportunity to achieve disease control
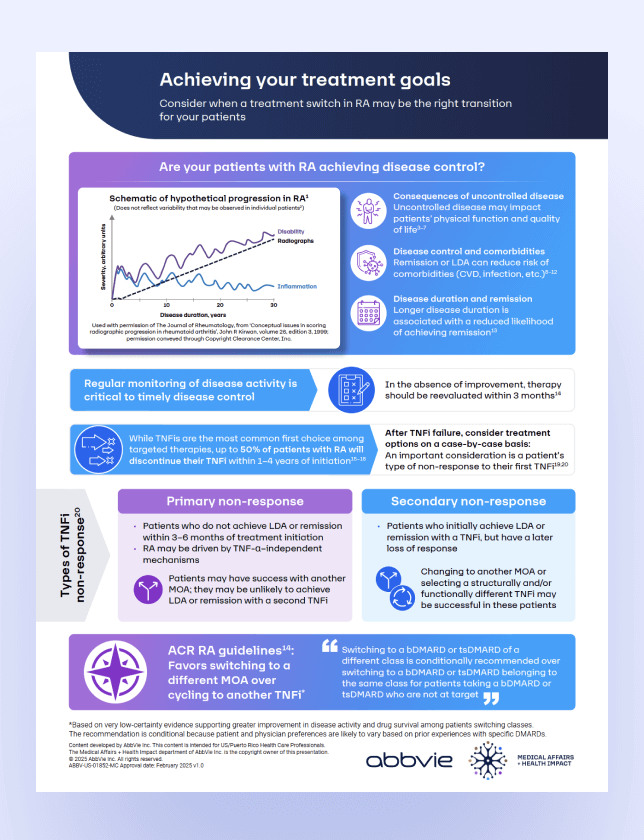
Consider when a treatment switch in RA may be the right transition for your patients
Resource
Learn more about when to consider a treatment switch: Downloadable infographic
Find additional details about the information reviewed here, as well as additional data to support your clinical decision-making
Learn more about when to consider a treatment switch: Downloadable infographic
Find additional details about the information reviewed here, as well as additional data to support you clinical decision-making

Explore more on RheumNow.com

Comorbidity risk in RA
Hear insights from Dr. Curtis and
Dr. Giles as they review additional data on the relationship between disease activity and comorbidity risk, including CVD and infection risk
Comorbidity risk in RA
Hear insights from Dr. Curtis and Dr. Giles as they review additional data on the relationship between disease activity and comorbidity risk, including CV and infection risk
Abbreviations:
ACR, American College of Rheumatology; ABA, abatacept; ADA, adalimumab; CVD, cardiovascular disease; DAS28, Disease Activity Score 28; DMARD, disease modifying antirheumatic drug; HAQ, health assessment questionnaire; IR-inadequate responder; LDA, low disease activity; MOA, mechanism of action; MTX, methotrexate; RA, rheumatoid arthritis; RCT, randomized controlled trial; TCZ, tocilizumab; TNFi, tumor necrosis factor inhibitor; UPA, upadacitinib; VAS, visual analog scale.
- Ajeganova S, Huizinga T. Ther Adv Musculoskelet Dis. 2017;9(10):249–262.
- Einarsson JT et al. J Rheumatol. 2016;43(6):1017–1023.
- Contreras-Yáñez I et al. BMC Musculoskelet Disord. 2017;18(1):379.
- McInnes IB, Schett G. N Engl J Med. 2011;365(23):2205–2219.
- Sokka T et al. Arthritis Res Ther. 2010;12(2):R42.
- Kim D et al. J Rheumatol. 2017;44(8):1112–1117.
- Kekow J et al. Rheumatology (Oxford). 2011;50(2):401–409.
- Myasoedova E et al. Ann Rheum Dis. 2016;75(3):560–565.
- Solomon DH et al. Arthritis Rheumatol. 2015;67(6):1449–1455.
- Mehta B et al. RMD Open. 2019;5(1):e000935.
- Listing J et al. Rheumatology (Oxford). 2013;52(1):53–61.
- Baecklund E et al. Arthritis Rheum. 2006;54(3):692–701.
- Fraenkel L et al. Arthritis Care Res (Hoboken). 2021;73(7):924–939.
- Migliore A et al. Ther Adv Musculoskelet Dis. 2021;13:1759720X211002682.
- Wei W et al. Adv Ther. 2017;34(8):1936–1952.
- Caporali R et al. Adv Ther. 2024;41(9):3706–3721.
- Perkins K et al. J Manag Care Spec Pharm. 2023;29(10-a Suppl.):M11.
- Bogas P et al. Ther Adv Musculoskelet Dis. 2021;13:1759720X211060910.
- Gottenberg JE et al. JAMA. 2016;316(11):1172–1180.
- Prevoo ML et al. Arthritis Rheum. 1995;38(1):44–48.
