Experts Discuss:
Treatment Decisions in Rheumatology and Gastroenterology
- 15-minute listen
Podcast

- Dr. Kathryn Dao & Dr. Amar Naik • December 2023
The experts

Kathryn Dao, MD
President, Rheum101
Rheumatologist
Dallas, TX

Amar Naik, MD
Associate Professor of Medicine
Director, Inflammatory Bowel Disease Program
Loyola Medicine
Key information
Cardiovascular disease1–3
Serious infection4–6
Malignancy7,8
Disease control may reduce background risk in RA and IBD9–14
Lifestyle (e.g., smoking and BMI), comorbidities, and medication can also impact risk7,9,15,16
Risk management
for
patients with chronic inflammatory disease
Disease control may help mitigate risk10,11,14: If disease is uncontrolled, consider switching to other treatment options
To mitigate the risk of serious infection, make sure patients are up-to-date on vaccinations, in accordance with the latest guidelines and the recommendations made in the prescribed product's labeling17
When making treatment decisions, consider17,18:
When making treatment decisions, carefully consider the patient’s complete medical history and individualized benefit vs risk of therapy17
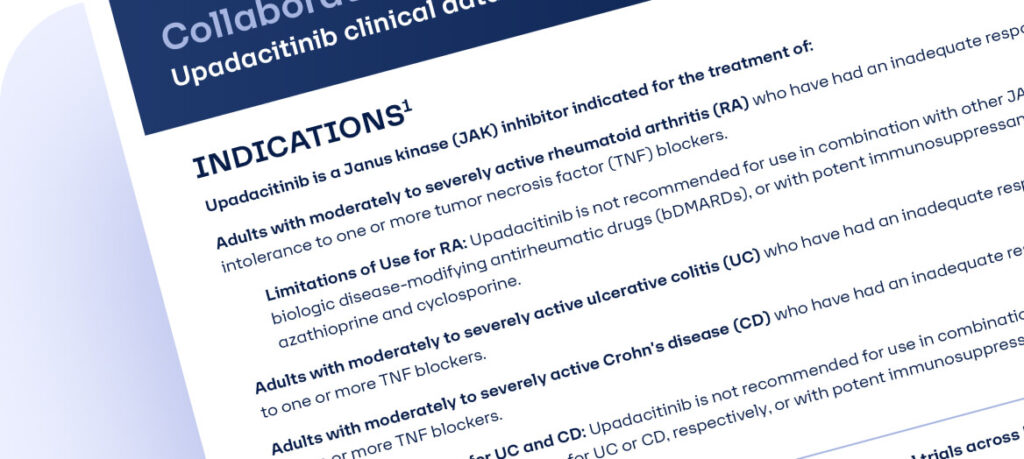
Resource
Learn about upadacitinib clinical studies in RA, UC, and CD
How often do you discuss background disease risk (CVD, serious infection, or malignancy) with your patients?
How important is disease control in your treatment strategy to control background risk?
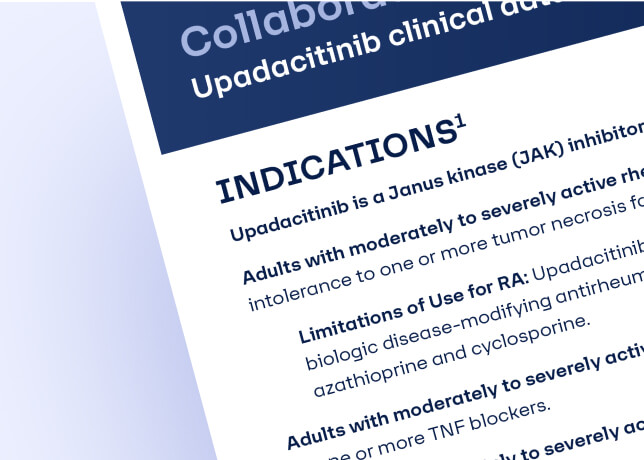
Indications
Important safety considerations and boxed warning
Serious Infections: Patients treated with upadacitinib are at increased risk for developing serious infections that may lead to hospitalization or death. These infections include tuberculosis (TB), invasive fungal, bacterial, viral, and other infections due to opportunistic pathogens. Most patients who developed these infections were taking concomitant immunosuppressants, such as methotrexate or corticosteroids. Test for latent TB before and during therapy; treat latent TB prior to use. Consider the risks and benefits prior to initiating therapy in patients with chronic or recurrent infection. If a serious infection develops, interrupt upadacitinib until the infection is controlled.
Mortality: In a postmarketing safety study in RA patients ≥ 50 years of age with at least one cardiovascular (CV) risk factor comparing another JAK inhibitor to TNF blockers, a higher rate of all-cause mortality, including sudden CV death, was observed with the JAK inhibitor.
Malignancies: Malignancies have been observed in upadacitinib treated patients. In RA patients treated with another JAK inhibitor, a higher rate of lymphomas and lung cancers was observed when compared with TNF blockers. Patients who are current or past smokers are at additional increased risk. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with upadacitinib, particularly in patients with a known malignancy (other than a successfully treated non-melanoma skin cancer [NMSC]), patients who develop a malignancy when on treatment, and patients who are current or past smokers. NMSCs have been reported in patients treated with upadacitinib. Periodic skin examination is recommended for patients who are at increased risk for skin cancer. Advise patients to limit sunlight exposure by wearing protective clothing and using sunscreen.
Major Adverse Cardiovascular Events (MACE): In RA patients who were ≥ 50 years of age with at least one CV risk factor treated with another JAK inhibitor, a higher rate of MACE (CV death, myocardial infarction, and stroke) was observed compared with TNF blockers. Patients who are current or past smokers are at additional increased risk. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with upadacitinib. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur. Discontinue upadacitinib in patients that have experienced a myocardial infarction or stroke.
Thrombosis: Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with JAK inhibitors, including upadacitinib. Many of these adverse events were serious and some resulted in death. In RA patients who were ≥ 50 years of age with at least one CV risk factor treated with another JAK inhibitor, a higher rate of thrombosis was observed when compared with TNF blockers. Avoid upadacitinib in patients at risk. Patients with symptoms of thrombosis should discontinue upadacitinib and be promptly evaluated.
Hypersensitivity Reactions: Upadacitinib is contraindicated in patients with known hypersensitivity to upadacitinib or any of its excipients. Serious hypersensitivity reactions such as anaphylaxis and angioedema were reported in patients receiving upadacitinib in clinical trials. If a clinically significant hypersensitivity reaction occurs, discontinue upadacitinib and institute appropriate therapy.
Other Serious Adverse Reactions: Patients treated with upadacitinib also may be at risk for other serious adverse reactions, including gastrointestinal perforations, neutropenia, lymphopenia, anemia, lipid elevations, liver enzyme elevations, and embryo-fetal toxicity.
Vaccinations: Avoid use of live vaccines during, or immediately prior to, upadacitinib therapy. Prior to initiating upadacitinib, it is recommended that patients be brought up to date with all immunizations, including varicella zoster or prophylactic herpes zoster vaccinations, in agreement with current immunization guidelines.
Medication Residue in Stool: Reports of medication residue in stool or ostomy output have occurred in patients taking upadacitinib. Most reports described patients with shortened gastrointestinal transit times. Instruct patients to contact their healthcare provider if medication residue is observed repeatedly.
Common Adverse Reactions in RA: The most common adverse reactions (≥1%) were upper respiratory tract infections, herpes zoster, herpes simplex, bronchitis, nausea, cough, pyrexia, acne, and headache.
Common Adverse Reactions in UC: The most common adverse reactions (≥5%) reported are upper respiratory tract infections, increased blood creatine phosphokinase, acne, neutropenia, elevated liver enzymes, and rash.
Common Adverse Reactions in CD: The most common adverse reactions (≥5%) reported are upper respiratory tract infections, anemia, pyrexia, acne, herpes zoster, and headache.
Review accompanying upadacitinib full Prescribing Information for additional information, visit www.rxabbvie.com or contact AbbVie Medical Information at 1-800-633-9110.
Explore more posts about patients with RA:

Heart to Heart: Experts Discuss Cardiovascular Risk in Rheumatoid Arthritis
Perspectives on the Safety of a JAK Inhibitor

Long-term JAK Inhibitor Treatment for Rheumatoid Arthritis (RA)
- van den Hoek J et al. Rheumatol Int. 2017;37(4):487–493.
- Conrad N et al. Lancet. 2022;300(10354):733–743.
- Aniwan S et al. Clin Gastroenterol Hepatol. 2018;16(10):1607–1615.
- Listing J et al. Rheumatology (Oxford). 2013;52(1):53–61.
- Lichtenstein GR et al. Am J Gastroenterol. 2012;107(9):1409–1422.
- Irving PM et al. BMJ Open Gastroenterol. 2021;8(1):e000573.
- De Cock D and Hyrich K. Best Pract Res Clin Rheumatol. 2018;32(6):869–886.
- Annese V et al. J Crohn’s Colitis. 2015;9(11):945–965.
- Solomon DH et al. Arthritis Rheumatol. 2015;67(8):1995–2003.
- Myasoedova E et al. Ann Rheum Dis. 2016;75(3):560–565.
- Accortt NA et al. Arthritis Care Res (Hoboken). 2018;70(5):679–684.
- Mehta B et al. RMD Open. 2019;5(1):e000935.
- Baecklund E et al. Arthritis Rheum. 2006;54(3):692–701.
- Kristensen SL et al. PLoS One. 2013;8(4):e56944.
- Crowson CS et al. Ann Rheum Dis. 2018;77(1):48–54.
- Crowson CS et al. Rheum Arthritis. 2012;64(9):2847–2855.
- Nash P et al. Ann Rheum Dis. 2021;80(1):71–87.
- Yang V et al. Drug Saf. 2023. Online ahead of print. doi: 10.1007/s40264-023-01333-0