
A JAKi Chat:
Shared Decision-Making in RA
- 20-minute listen
Podcast
- Dr. Curtis & Dr. Winthrop • October 2025
The experts
Jeffrey R. Curtis, MD, MS, MPH
Professor of Medicine, Epidemiology, and Computer Science
Division of Clinical Immunology and Rheumatology
University of Alabama at Birmingham

Kevin Winthrop, MD, MPH
Professor
School of Medicine,
Divisions of Infectious
Diseases and Ophthalmology
School of Public Health
Oregon Health and Sciences University
NEW Upadacitinib
Digital Data Guide
Use the guide discussed in the podcast to explore key efficacy data and ~8.5 years of safety data from the RA Phase 3 program
Learn more about
UPA in RA:
Only for use by healthcare providers.
How are you talking
about risk in RA?
In the podcast, Dr. Curtis and Dr. Winthrop share how they talk to patients about RA and their treatment options.
Talk about the impact of uncontrolled RA
Patients with uncontrolled RA have been observed to have an increased risk of CV disease, infection, and malignancy1-5
Consider modifiable risk factors
How could smoking cessation or vaccination lower your patient’s risk?
Discuss the benefits and risks of different treatments
Inform your patients regarding treatment efficacy and safety
Tips on shared decision-making from Dr. Curtis and Dr. Winthrop6
Remember to have a CHAT with your patients:
Consider your patient’s understanding and context,
and meet them where they’re at
Highlight medication risk
by sharing important safety content
Anchor to your patient's baseline risk
for outcomes related to the disease itself and other risk factors (e.g. comorbidities)
Tune in to your patient's motivation and emotions,
and commit to continued discussions
Learn more about the art of shared decision-making
Click the link to see the paper co-authored by Dr. Curtis and read additional recommendations for communicating benefit and risk to patients with RA.
CHAT with your patients with RA
so they can engage in more informed shared treatment decisions.
CV, cardiovascular; EULAR, European Alliance of Associations for Rheumatology; JAKi, Janus kinase inhibitor; MOA, mechanism of action; RA, rheumatoid arthritis; TNFi, tumor necrosis factor inhibitor; UPA, upadacitinib.
INDICATION
Adults with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response or intolerance to one or more tumor necrosis factor (TNF) blockers.
Limitations of Use for RA: Upadacitinib is not recommended for use in combination with other JAK inhibitors, biologic disease-modifying antirheumatic drugs (bDMARDs), or with potent immunosuppressants such as azathioprine and cyclosporine.
Important safety considerations and boxed warning
Serious Infections: Patients treated with upadacitinib are at increased risk for developing serious infections that may lead to hospitalization or death. These infections include tuberculosis (TB), invasive fungal, bacterial, viral, and other infections due to opportunistic pathogens. Most patients who developed these infections were taking concomitant immunosuppressants, such as methotrexate or corticosteroids. Test for latent TB before and during therapy; treat latent TB prior to use. Consider the risks and benefits prior to initiating therapy in patients with chronic or recurrent infection. If a serious infection develops, interrupt upadacitinib until the infection is controlled.
Mortality: In a postmarketing safety study in RA patients ≥50 years of age with at least one cardiovascular (CV) risk factor comparing another JAK inhibitor to TNF blockers, a higher rate of all-cause mortality, including sudden CV death, was observed with the JAK inhibitor.
Malignancies: Malignancies have been observed in upadacitinib treated patients. In RA patients treated with another JAK inhibitor, a higher rate of lymphomas and lung cancers was observed when compared with TNF blockers. Patients who are current or past smokers are at additional increased risk. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with upadacitinib, particularly in patients with a known malignancy (other than a successfully treated non-melanoma skin cancer [NMSC]), patients who develop a malignancy when on treatment, and patients who are current or past smokers. NMSCs have been reported in patients treated with upadacitinib. Periodic skin examination is recommended for patients who are at increased risk for skin cancer. Advise patients to limit sunlight exposure by wearing protective clothing and using sunscreen.
Major Adverse Cardiovascular Events (MACE): In RA patients who were ≥50 years of age with at least one CV risk factor treated with another JAK inhibitor, a higher rate of MACE (CV death, myocardial infarction, and stroke) was observed compared with TNF blockers. Patients who are current or past smokers are at additional increased risk. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with upadacitinib. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur. Discontinue upadacitinib in patients that have experienced a myocardial infarction or stroke.
Thrombosis: Thromboses, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with JAK inhibitors, including upadacitinib. Many of these adverse events were serious and some resulted in death. In RA patients who were ≥50 years of age with at least one CV risk factor treated with another JAK inhibitor, a higher rate of thrombosis was observed when compared with TNF blockers. Avoid upadacitinib in patients at risk. Patients with symptoms of thrombosis should discontinue upadacitinib and be promptly evaluated.
Hypersensitivity Reactions: Upadacitinib is contraindicated in patients with known hypersensitivity to upadacitinib or any of its excipients. Serious hypersensitivity reactions such as anaphylaxis and angioedema were reported in patients receiving upadacitinib in clinical trials. If a clinically significant hypersensitivity reaction occurs, discontinue upadacitinib and institute appropriate therapy.
Other Serious Adverse Reactions: Patients treated with upadacitinib also may be at risk for other serious adverse reactions, including gastrointestinal perforations, neutropenia, lymphopenia, anemia, lipid elevations, liver enzyme elevations, and embryo-fetal toxicity. If upadacitinib exposure occurs during pregnancy, please report the pregnancy to the surveillance program by calling 1-800-633-9110.
Vaccinations: Avoid use of live vaccines during, or immediately prior to, upadacitinib therapy. Prior to initiating upadacitinib, it is recommended that patients be brought up to date with all immunizations, including prophylactic varicella zoster or herpes zoster vaccinations, in agreement with current immunization guidelines.
Medication Residue in Stool: Reports of medication residue in stool or ostomy output have occurred in patients taking upadacitinib extended-release tablet. Most reports described patients with shortened gastrointestinal transit times. Instruct patients to contact their healthcare provider if medication residue is observed repeatedly.
Common Adverse Reactions in RA: The most common adverse reactions (≥1%) were upper respiratory tract infections, herpes zoster, herpes simplex, bronchitis, nausea, cough, pyrexia, acne, and headache.
Review accompanying upadacitinib full Prescribing Information for additional information, visit www.rxabbvie.com or contact AbbVie Medical Information at 1-800-633-9110.
Explore related topics on RheumNow.com

Treatment goals for RA: Is it time to transition MOAs?
Rheumatologists Dr. Christina Charles-Schoeman and Dr. Manish Jain discuss their approaches to setting and pursuing treatment goals for patients with poorly controlled RA after TNFis

RA Risk Radar: Heart Disease, Infection, and Malignancy
Rheumatologists Dr. Jeffrey Curtis and Dr. Jon Giles discuss the risk of comorbidities that can occur as a consequence of uncontrolled inflammation in RA
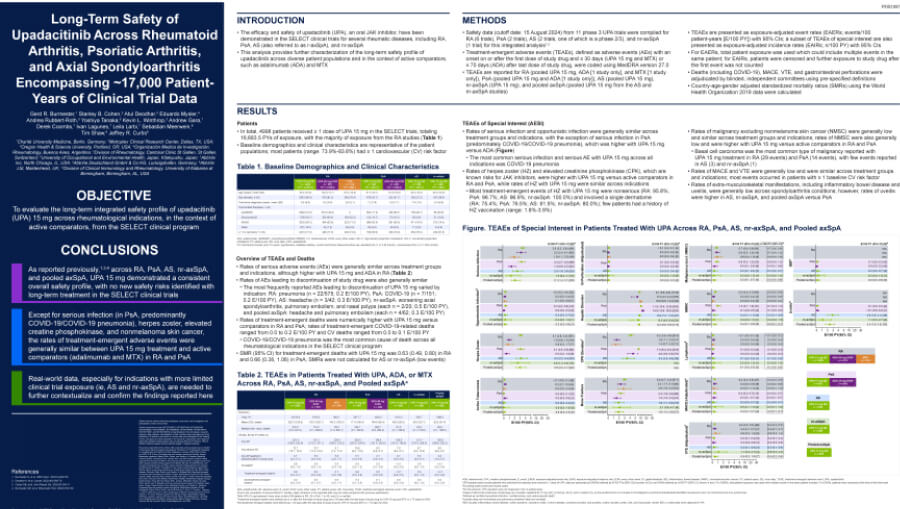
Long-term safety of a JAKi across ~17,000 patient-years
Presented at EULAR 2025, this poster examines the long-term safety of UPA across multiple Phase 3 trials
Treatment goals for RA: Is it time to transition MOAs?
Rheumatologists Dr. Christina Charles-Schoeman and Dr. Manish Jain discuss their approaches to setting and pursuing treatment goals for patients with poorly controlled RA after TNFis
RA Risk Radar: Heart Disease, Infection, and Malignancy
Rheumatologists Dr. Jeffrey Curtis and Dr. Jon Giles discuss the risk of comorbidities that can occur as a consequence of uncontrolled inflammation in RA
Long-term safety of a JAKi across ~17,000 patient-years
Presented at EULAR 2025, this poster examines the long-term safety of UPA across multiple Phase 3 trials
- Myasoedova E et al. Ann Rheum Dis. 2016;75(3):560-565.
- Mehta B et al. RMD Open. 2019;5(1):e000935.
- Yun H et al. Arthritis Care Res (Hoboken). 2023;75(8):1639-1647.
- Hellgren K et al. Arthritis Rheumatol. 2017;69(4):700-708.
- Baecklund E et al. Arthritis Rheum. 2006;54(3):692-701.
- Curtis JR, Fraenkel L. Arthritis Rheumatol. 2024;76(4):493-496.
The AbbVie Medical Affairs + Health Impact department of AbbVie Inc. is the copyright owner of this presentation and has paid RheumNow to host this content. AbbVie is solely responsible for all written content within this presentation.
